金桔
金币
威望
贡献
回帖0
精华
在线时间 小时
|
登陆有奖并可浏览互动!
您需要 登录 才可以下载或查看,没有账号?立即注册


×

Minimal residual disease as a target for liquid biopsy in patients with solid tumours 将微小残留病灶作为实体瘤患者液体活检的目标
Abstract 摘要
转移是实体瘤患者死于癌症的主要原因。目前的成像技术还不足以灵敏地检测出初次手术或化疗后的微小残留病灶(MRD,又称可测量或分子残留病灶),因此需要更灵敏的检测方法来检测体内残留的癌症痕迹。
Metastasis is the leading cause of cancer-related death in patients with solid tumours. Current imaging technologies are not sufficiently sensitive to detect minimal residual disease (MRD; also known as measurable or molecular residual disease) after initial surgery or chemotherapy, pointing to the need for more sensitive tests to detect remaining traces of cancer in the body.
液体活检,即分析血液或其他体液中的肿瘤衍生细胞或肿瘤诱导细胞或细胞产物,为检测和监测MRD开辟了一条新的诊断途径。液体活检已被用于血液恶性肿瘤患者的临床决策。在此我们回顾了目前利用循环肿瘤DNA(ctDNA)检测和监测实体瘤患者MRD的知识。
Liquid biopsy, or the analysis of tumour-derived or tumour-induced cells or cellular products in the blood or other body fluids, has opened a new diagnostic avenue to detect and monitor MRD. Liquid biopsy is already used in clinical decision making for patients with haematological malignancies. Here, we review current knowledge on the use of circulating tumour DNA (ctDNA) to detect and monitor MRD in patients with solid tumours.
我们还讨论了ctDNA引导下的MRD检测和特征描述如何预示着新时代的“辅助后疗法 ”,这种疗法有可能在影像学显示终末转移性疾病之前消除MRD并治愈患者。
We also discuss how ctDNA-guided MRD detection and characterization could herald a new era of novel‘post-adjuvant therapies’ with the potential to eliminate MRD and cure patients before terminal metastatic disease is evident on imaging.
综述要点 Key points
- 灵敏的血液化验可检测极低浓度(低至 <10 ppm)的循环肿瘤 DNA (ctDNA)。Sensitive blood assays enable the detection of circulating tumour DNA (ctDNA) at very low concentrations (down to <10 ppm).
- 要检测实体瘤患者的微小残留病灶(MRD,又称可测量或分子残留病灶),就必须检测极低浓度的ctDNA。The detection of very low concentrations of ctDNA is required to detect minimal residual disease (MRD; also known as measurable or molecular residual disease) in patients with solid tumours.
- 微小残留病灶MRD检测可与无进展生存期和总生存期等临床结果相关联。MRD detection can be correlated with clinical outcomes such as progression-free survival and overall survival.
- 基于ctDNA的微小残留病灶MRD检测可比基于影像学的复发检测早几个月,这取决于肿瘤的类型和分期。ctDNA-based MRD detection can precede imaging-based detection of relapse by several months depending on the tumour type and stage.
- ctDNA检测到的微小残留病灶MRD向明显转移的转变取决于残余肿瘤负荷TMB和宿主反应(如抗肿瘤免疫)。The transition of ctDNA-detectable MRD to overt metastasis can depend on the residual tumour burden and the host response (for example, antitumour immunity)。
- 目前需要对实体瘤 MRD微小残留病灶 阳性患者进行干预性临床研究,以评估哪种治疗方法可以消除这些患者的微小残留病灶MRD。Interventional clinical studies in patients with solid tumours and MRD positivity are now required to assess which treatment(s) can eliminate MRD in these patients。
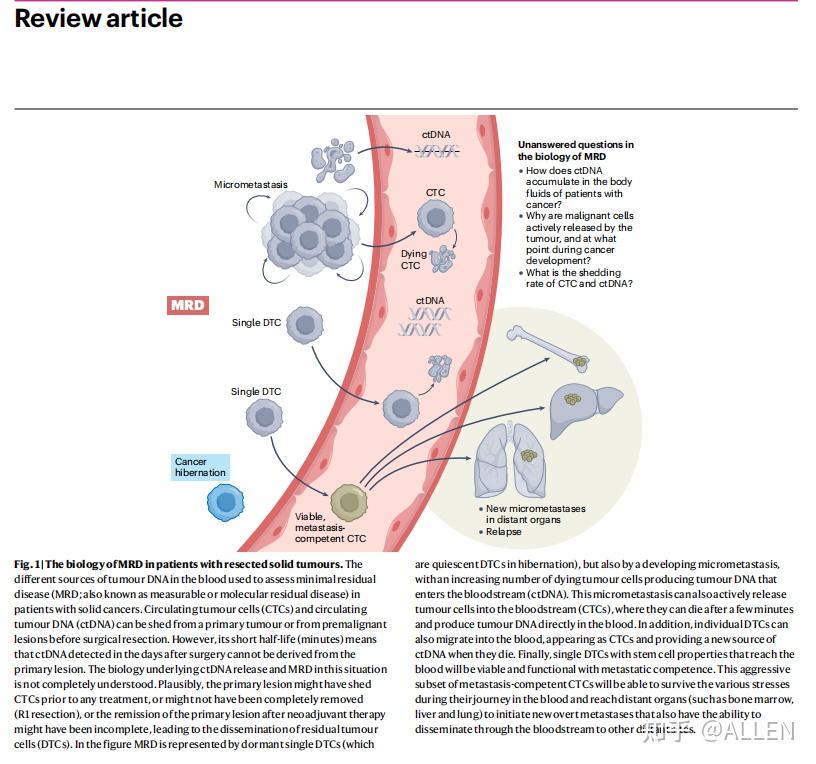
图 1:患者切除实体瘤后微小残留病灶MRD生物学特性。
The different sources of tumour DNA in the blood used to assess minimal residual disease (MRD; also known as measurable or molecular residual disease) in patients with solid cancers.
血液中实体瘤患者肿瘤 DNA 的不同来源,用于评估切除实体瘤患者的最小残留病灶(MRD;也称为可测量或分子微小残留病灶)。
Circulating tumour cells (CTCs) and circulating tumour DNA (ctDNA) can be shed from a primary tumour or from premalignant lesions before surgical resection. However, its short half-life (minutes) means that ctDNA detected in the days after surgery cannot be derived from the primary lesion.
循环肿瘤细胞(CTCs)和循环肿瘤 DNA(ctDNA)可在手术切除前从原发肿瘤或恶性前病变中脱落。然而,由于其半衰期很短(几分钟),因此术后几天内检测到的 ctDNA 不可能来自原发病灶。
The biology underlying ctDNA release and MRD in this situation is not completely understood. Plausibly, the primary lesion might have shed CTCs prior to any treatment, or might not have been completely removed (R1 resection), or the remission of the primary lesion after neoadjuvant therapy might have been incomplete, leading to the dissemination of residual tumour cells (DTCs).
在这种情况下,ctDNA 释放和 MRD 的生物学基础尚不完全清楚。原发病灶可能在任何治疗之前就已经脱落了 CTCs,或可能在手术后数天仍未完全切除。新辅助治疗后原发病灶未完全缓解,导致残余肿瘤细胞(DTCs 细胞)。
In the figure MRD is represented by dormant single DTCs (which are quiescent DTCs in hibernation), but also by a developing micrometastasis, with an increasing number of dying tumour cells producing tumour DNA that enters the bloodstream (ctDNA).
在图中,MRD 表现为休眠的单个 DTC(即处于休眠状态的 DTC),也表现为随着越来越多的肿瘤细胞死亡导致发展中的微转移,这种微转移也会主动释放肿瘤细胞到血液中(ctDNA)。
This micrometastasis can also actively release tumour cells into the bloodstream (CTCs), where they can die after a few minutes and produce tumour DNA directly in the blood.
肿瘤细胞(CTCs)会在几分钟后死亡,并直接在血液中产生肿瘤 DNA。
In addition, individual DTCs can also migrate into the blood, appearing as CTCs and providing a new source of ctDNA when they die.
此外,单个 DTC 也会迁移到血液中,以 CTCs 的形式出现,并在死亡后提供新的 ctDNA 来源。
Finally, single DTCs with stem cell properties that reach the blood will be viable and functional with metastatic competence.
最后,进入血液的具有干细胞特性的单个DTC 具有转移能力。
This aggressive subset of metastasis-competent CTCs will be able to survive the various stresses during their journey in the blood and reach distant organs (such as bone marrow, liver and lung) to initiate new overt metastases that also have the ability to disseminate through the bloodstream to other distant sites.
这种具有侵袭性的转移能力的 CTC 亚群将能在血液中的各种压力下存活下来到达血液中,并到达远处的器官(如骨髓、肝脏和肺部),从而引发新的明显转移灶,这些转移灶还能通过血液传播到其他远处部位。
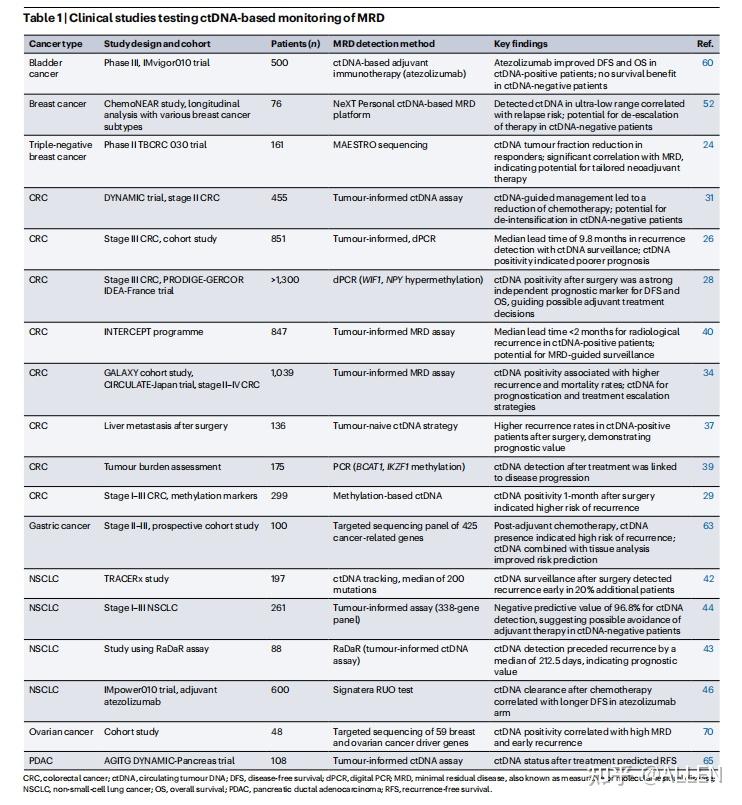
表 1 基于ctDNA的 MRD 监测的临床研究 Table 1 | Clinical studies testing ctDNA-based monitoring of MRD
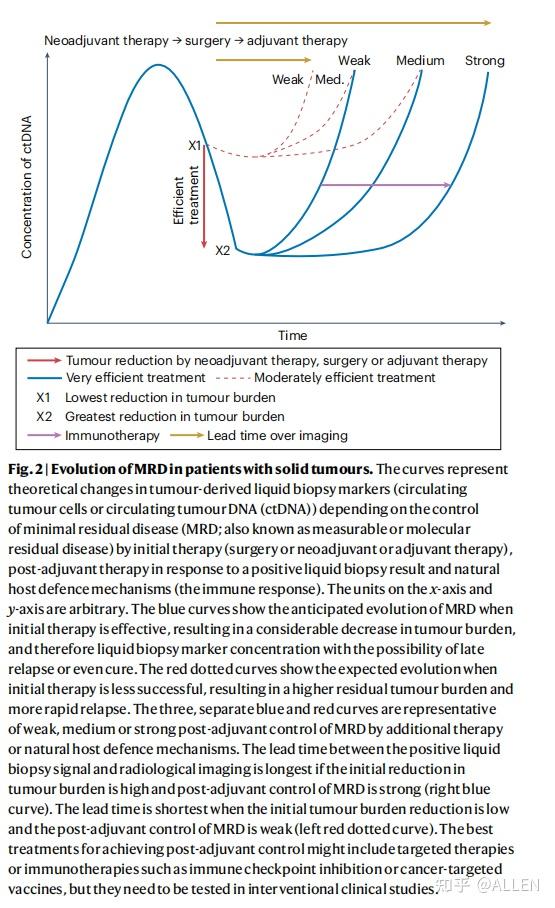
Fig. 2 | Evolution of MRD in patients with solid tumours. 图 2:实体瘤患者的微小残留病灶MRD 的变化。
The curves represent theoretical changes in tumour-derived liquid biopsy markers (circulating tumour cells or circulating tumour DNA (ctDNA)) depending on the control of minimal residual disease (MRD; also known as measurable or molecular residual disease) by initial therapy (surgery or neoadjuvant or adjuvant therapy), post-adjuvant therapy in response to a positive liquid biopsy result and natural host defence mechanisms (the immune response).
曲线代表肿瘤衍生液体活检标志物(循环肿瘤细胞或ctDNA循环肿瘤DNA )的理论变化,这取决于手术或新辅助治疗或辅助治疗对极小残留病(MRD,又称可测量或分子残留病)的控制情况、辅助治疗后对阳性液体活检结果的反应,以及自然宿主防御机制(免疫反应)。
The units on the x-axis and y-axis are arbitrary. The blue curves show the anticipated evolution of MRD when initial therapy is effective, resulting in a considerable decrease in tumour burden, and therefore liquid biopsy marker concentration with the possibility of late relapse or even cure.
x 和y轴的单位是随意的。蓝色曲线显示了初始治疗有效时 MRD 的预期变化。如果初始治疗有效,肿瘤负荷大幅减少、因此液体活检标记物浓度也会大大降低,有可能表示更晚期的复发,甚至代表了治愈的可能性。
The red dotted curves show the expected evolution when initial therapy is less successful, resulting in a higher residual tumour burden and more rapid relapse.
红色虚线显示的是初始治疗效果不佳时的预期变化情况,导致残余肿瘤负荷增加,复发速度加快。
The three, separate blue and red curves are representative of weak, medium or strong post-adjuvant control of MRD by additional therapy or natural host defence mechanisms.
三条独立的蓝色和红色曲线分别代表,通过额外治疗或自然宿主防御机制对MRD进行弱、中或强的辅助治疗后控制。
The lead time between the positive liquid biopsy signal and radiological imaging is longest if the initial reduction in tumour burden is high and post-adjuvant control of MRD is strong (right blue curve).
如果最初的肿瘤负荷减少较多,且辅助治疗后对 MRD 的控制较强,则液体活检阳性信号与放射成像之间的前导间隔时间最长(右蓝曲线)。
The lead time is shortest when the initial tumour burden reduction is low and the post-adjuvant control of MRD is weak (left red dotted curve).
如果最初的肿瘤负荷降低程度较低,而辅助治疗后的 MRD 控制较强,则前导间隔时间最短(左侧红色虚线)。
The best treatments for achieving post-adjuvant control might include targeted therapies or immunotherapies such as immune checkpoint inhibition or cancer-targeted vaccines, but they need to be tested in interventional clinical studies.
最佳实现辅助治疗后控制的最佳疗法可能包括靶向疗法或免疫疗法,如免疫检查点抑制或癌症靶向疫苗,但它们需要在介入性临床研究中进行测试。
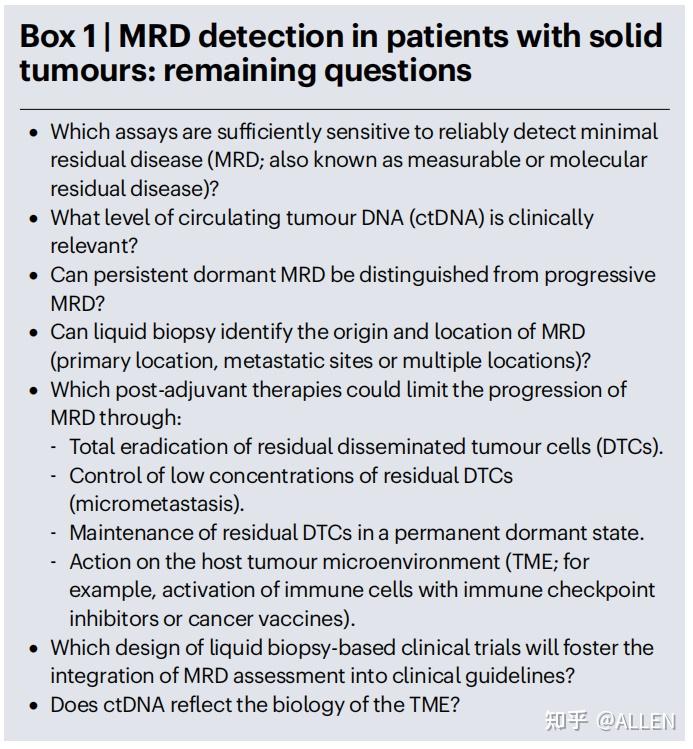
方框 1 实体瘤患者的 MRD 检测:尚存的问题 Box 1 | MRD detection in patients with solid tumours: remaining questions
Box 1 实体瘤患者的 MRD 检测:尚存的问题
• 哪些检测方法具有足够的灵敏度,能够可靠地检测出MRD微小残留病灶?Which assays are suficiently sensitive to reliably detect minimal residual disease (MRD; also known as measurable or molecular residual disease)?
• 何种水平的循环肿瘤 DNA(ctDNA)具有临床意义? What level of circulating tumour DNA (ctDNA) is clinically relevant?
• 能否将持续休眠的 MRD 与进展性 MRD 区分开来?Can persistent dormant MRD be distinguished from progressive MRD?
• 液体活检能否确定 MRD 的来源和位置?(原发部位、转移部位或多个部位)?Can liquid biopsy identify the origin and location of MRD (primary location, metastatic sites or multiple locations)?
• 哪些辅助后疗法可以通过以下方式限制 MRD 的进展?Which post-adjuvant therapies could limit the progression of MRD through:
- 彻底根除残留的播散性肿瘤细胞(DTCs)。 Total eradication of residual disseminated tumour cells (DTCs).
- 控制低浓度的残留扩散肿瘤细胞(微转移)。Control of low concentrations of residual DTCs
(micrometastasis).
- 使残留的 DTC 保持永久休眠状态。Maintenance of residual DTCs in a permanent dormant state.
- 对宿主肿瘤微环境(TME)产生作用,例如用免疫检查点抑制剂,或癌症疫苗激活免疫细胞)。Action on the host tumour microenvironment (TME; for example, activation of immune cells with immune checkpoint inhibitors or cancer vaccines).
• 基于液体活检的临床试验的设计将促进将MRD评估纳入临床指南?Which design of liquid biopsy-based clinical trials will foster the integration of MRD assessment into clinical guidelines?
• ctDNA能否反映TME的生物学特性? Does ctDNA reflect the biology of the TME?

Box 2 | Control of MRD 方框 2 MRD 的控制
Box 2 MRD 的控制
• 控制微小残留病灶(MRD,也称为可测量或分子残留病灶)需要将极早期检测、针对 MRD 的专用疗法、监测和支持性护理相结合,目的是改善患者预后和预防癌症复发。 Control of minimal residual disease (MRD; also known as measurable or molecular residual disease) requires a combination of very early detection, dedicated MRD-targeted therapies, surveillance and supportive care, with the aim of improving patient outcomes and preventing cancer relapse.
• 除了残留扩散肿瘤细胞的负荷和分子特征外分子特征外,还可以通过液体活检对宿主对 MRD 的反应进行平行评估。液态活检分析对宿主对 MRD 的反应至关重要。了解和预防 MRD 进展为明显转移至关重要。In addition to the burden and molecular characteristics of residual disseminated tumour cells, parallel assessment of the host response to MRD by liquid biopsy analysis could be crucial in understanding and preventing MRD progression to overt metastasis.
• 免疫系统对于识别和消灭癌细胞至关重要。改善免疫监视是控制 MRD 的有效技术。目前正在研究免疫检查点抑制剂、嵌合抗原受体T细胞疗法和癌症疫苗, 可改善对 MRD 的自然免疫反应。The immune system is essential to the recognition and destruction of cancer cells. Improving immune surveillance can be an efective technique for controlling MRD. Immune-checkpoint inhibitors, chimeric antigen receptor T cell therapy and cancer vaccines are being investigated to improve the natural immune response to MRD.
• 检测 MRD 的新方法以液体活检为基础,提高了追踪新出现克隆的灵敏度。新的 MRD 控制方法包括:New methods of detecting MRD, based on liquid biopsy with enhanced sensitivity to trace emerging clones, are being explored and novel approaches to MRD control include:
- 从不同角度同时针对 MRD 的综合疗法。- Combination therapies to simultaneously target MRD from various angles.
- 根据每位患者 MRD 的基因和分子特征进行个性化治疗。- Personalized medicine based on the genetic and molecular profile of MRD in each patient.
参考文献
Pantel, K., Alix-Panabières, C. Minimal residual disease as a target for liquid biopsy in patients with solid tumours. Nat Rev Clin Oncol 22, 65–77 (2025). https://doi.org/10.1038/s41571-024-00967-y
https://www.nature.com/articles/s41571-024-00967-y
原文地址:https://zhuanlan.zhihu.com/p/14001404515 |
|
 /3
/3 